Breathing Techniques for Pain Relief and Anxiety After Injury
Pain and anxiety after injury affect both the body and the nervous system. Discover gentle, science-informed breathing techniques that calm the nervous system, reduce pain sensitivity, and support recovery. Learn practical practices you can use safely at home, guided by the trauma-aware approach of ValU Within Mindful Studio in Murcia.
Gentle nervous system support for recovery, safety, and emotional balance
Pain after an injury is not only physical. It affects the nervous system, sleep, emotions, and confidence in your own body. Many people notice that when pain appears, their breathing becomes shallow, tense, or irregular — which can actually intensify pain and anxiety.
The good news:
Simple breathing practices can help calm the nervous system, reduce pain sensitivity, and restore a sense of safety in the body.
These techniques are gentle, accessible, and can be practiced seated or lying down, as long as your position is safe and comfortable.
Important: These practices are for education and self-regulation support. They do not replace medical care. If you feel dizzy, short of breath, or your pain worsens, stop and consult your healthcare professional.
Why breathing helps with pain and recovery
Scientific research shows that slow, controlled breathing can:
• Activate the parasympathetic nervous system (“rest and repair” mode)
• Reduce stress hormones such as cortisol
• Lower muscle tension
• Improve oxygen delivery to tissues
• Reduce pain perception in the brain
• Improve sleep quality
• Decrease anxiety and emotional overwhelm
Sources include:
• National Health Service (NHS, UK)
• British Heart Foundation
• Cleveland Clinic
• PubMed Central (NIH studies on breathwork and pain modulation)
• Center for Clinical Interventions (CCI, Australia)
1. Diaphragmatic (Belly) Breathing
This is the foundation of all calming breath practices and especially helpful when pain causes shallow breathing.
How to practice:
1. Sit or lie comfortably (knees bent if on your back).
2. Place one hand on your chest and one on your belly.
3. Inhale slowly through the nose so the belly rises more than the chest.
4. Exhale gently, letting the belly soften.
5. Continue for 5–10 breaths (2–5 minutes).
You may also imagine breathing towards the painful area on the inhale and softening around it on the exhale. This helps the brain reduce threat signals around pain.
2. Box Breathing (4–4–4–4)
This technique offers structure and mental focus, which is especially helpful when anxiety feels overwhelming.
Pattern:
• Inhale 4
• Hold 4
• Exhale 4
• Hold 4
• Repeat for 4–8 rounds
If this feels too strong, use shorter counts (3–3–3–3). This technique is supported by organizations like the British Heart Foundation and used widely for stress regulation.
3. 4–7–8 Calming Breath
Often called a “natural sedative for the nervous system,” this breath is useful at night, during pain flare-ups, or emotional overwhelm.
How to practice:
1. Exhale fully through the mouth
2. Inhale through the nose for 4
3. Hold for 7 (shorter if uncomfortable)
4. Exhale slowly through the mouth for 8
5. Repeat 3–4 cycles
This technique was popularized by Dr. Andrew Weil and is widely used in sleep and anxiety support.
4. Pursed-Lip Breathing (For tension and breath-holding)
When pain causes people to hold their breath (very common!), this technique helps regulate breathing rhythm.
Practice:
• Inhale gently through the nose (2 counts)
• Exhale slowly through softly pursed lips (4+ counts)
• Continue for a few minutes
This method is also used in clinical respiratory therapy and recommended by medical organizations such as the NHS and Cleveland Clinic.
5. Mindful Breathing with Pain-Focused Imagery
This approach combines breath with gentle attention, helping the brain reinterpret pain signals.
How to practice:
1. Begin with slow belly breathing
2. Bring awareness to the painful area without judgment
3. Inhale imagining warmth and space entering the area
4. Exhale imagining tension leaving
5. Practice for 3–5 minutes
This method is supported by pain psychology research (including studies published in PubMed Central and clinical programs like CCI Australia).
How often should you practice?
For best results:
• 5–10 minutes once or twice daily
• Plus a few slow breaths whenever pain or anxiety spikes
• Practice at consistent times (morning and evening work well)
Stop if you feel:
• Dizzy
• Air-hungry
• Increased pain
• Chest discomfort
Always choose positions approved by your doctor or physiotherapist during early recovery.
A gentle message if you’re recovering
If you’re experiencing pain, frustration, or loss of trust in your body — you’re not weak. Your nervous system is simply trying to protect you. These breathing practices are not about forcing healing, but about creating the inner conditions where healing becomes possible.
At ValU Within Mindful Studio in Lo Santiago (Murcia), we integrate breath-based practices into gentle yoga, restorative sessions, and nervous system regulation classes specifically designed for adults 40+, injury recovery, and life transitions.
Yoga for post-accident recovery: gentle healing for body and mind.
Discover how gentle yoga can support recovery after an accident. Improve mobility, reduce pain, calm the nervous system, and rebuild confidence in your body safely with guided, trauma-informed practices.
HOW YOGA SUPPORTS RECOVERY AFTER AN ACCIDENT
Recovering from an accident—such as fractures, sprains, surgeries, or brain injuries—can be physically and emotionally challenging. While medical care and physiotherapy are essential, yoga offers a gentle, effective complement. Practiced safely, it supports physical healing, nervous system balance, and emotional recovery.
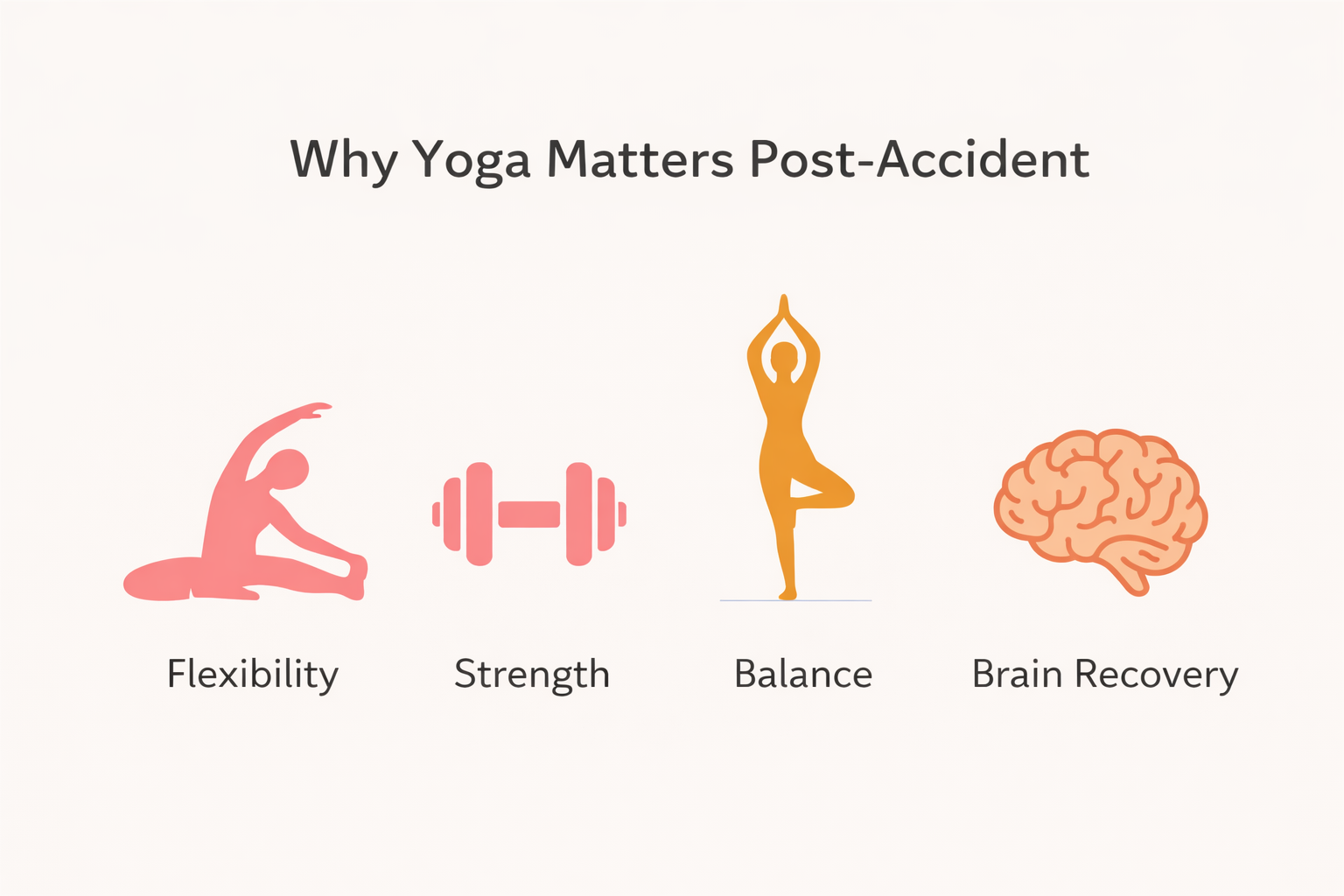
WHY YOGA HELPS AFTER AN ACCIDENT
Yoga is more than flexibility and strength—it reconnects your body, breath, and mind. After an accident, yoga can:
Improve flexibility, strength, and balance: Key factors in rehabilitation and returning to daily activities or sports.
Enhance joint mobility and muscle control: Gentle asanas (postures) support recovery from sprains, strains, and orthopedic injuries.
Support brain injury and stroke recovery: Adapted yoga has been linked to better motor function, balance, and quality of life.
Rebuild confidence in movement: Slow, mindful practice helps reduce fear of movement often experienced after trauma.
YOGA FOR PAIN RELIEF AND NERVOUS SYSTEM REGULATION
Yoga has well-documented effects on pain management and nervous system function:
Reduces chronic pain: Yoga benefits people with low back pain, arthritis, and musculoskeletal issues that may worsen post-accident.
Activates the parasympathetic nervous system: Gentle movement and breathwork trigger the “rest and digest” response, calming the body.
Stimulates the vagus nerve: Improves breath depth, lowers heart rate, and eases muscle tension, reducing anxiety and hypervigilance.
Supports trauma recovery: Regular practice can reduce intrusive thoughts, hyperarousal, and emotional reactivity.
EMOTIONAL AND PSYCHOLOGICAL BENEFITS OF YOGA AFTER AN ACCIDENT
Accidents can impact mental health, leading to stress, anxiety, PTSD, or sleep disturbances. Yoga supports emotional recovery by:
Reducing PTSD symptoms and improving mood: Yoga-based programs enhance mental well-being.
Encouraging mindfulness and body awareness: Notice sensations and emotions without becoming overwhelmed.
Restoring a sense of safety in the body: Gradual reconnection after pain or immobilization rebuilds trust in movement.
Simple grounding exercises: Seated breathing paired with a body scan—feeling your feet on the floor or the chair beneath—can gently reconnect you with your body.
PRACTICAL WAYS TO INTEGRATE YOGA INTO REHABILITATION
To safely use yoga after an accident:
Start with gentle breathwork and relaxation: Diaphragmatic breathing, short box breathing, and small, pain-free movements.
Use props and support: Chairs, walls, and yoga props help improve mobility, posture, and balance safely.
Focus on targeted poses: Core, hips, and hamstrings support stability, flexibility, and injury prevention.
Follow trauma-informed yoga: Slow pacing, choice, and non-triggering language are ideal for emotional healing.
SAFETY CONSIDERATIONS FOR POST-ACCIDENT YOGA
Safety is essential to avoid further injury:
Get medical clearance: Always consult your doctor before starting yoga after fractures, surgery, or serious injuries.
Modify or avoid risky poses: Conditions like glaucoma, osteoporosis, hernia, recent joint replacement, uncontrolled blood pressure, or pelvic floor injuries require adaptation. Avoid deep forward bends, intense core compression, weight-bearing, or head-below-heart positions unless cleared.
Avoid extreme practices: Headstands and forceful breathing are high-risk, especially for beginners or those in rehabilitation.
Work with a qualified instructor: A yoga therapist or experienced teacher can guide you safely within a pain-free range.
CONCLUSION
Yoga can be a powerful tool in post-accident recovery. It supports physical rehabilitation, reduces pain, regulates the nervous system, and aids emotional healing. With gentle, guided practice, yoga helps you rebuild confidence, regain mobility, and restore balance in both body and mind.
Releasing joint pain during menopause: finding ease through breath, meditation, and yoga
Releasing Joint Pain During Menopause: Finding Ease Through Breath, Meditation, and Yoga
Many women expect hot flashes and mood swings during menopause—but joint pain often comes as a surprise. Suddenly, knees feel stiff in the morning, hips ache after sitting, or shoulders tighten for no reason. Research shows that up to half of women in menopause experience joint pain, yet it is rarely talked about.
The cause? Changing hormone levels. As estrogen declines, the body produces less collagen and joint lubrication, which can lead to inflammation and stiffness. Add in stress, sleep changes, or simply the natural wear and tear of life, and our joints begin to speak up.
But here’s the good news: you can take back comfort. With a few mindful practices—alongside healthy lifestyle choices—joint pain can be eased, and movement can feel light and joyful again.
Many women expect hot flashes and mood swings during menopause—but joint pain often comes as a surprise. Suddenly, knees feel stiff in the morning, hips ache after sitting, or shoulders tighten for no reason. Research shows that up to half of women in menopause experience joint pain, yet it is rarely talked about.
The cause? Changing hormone levels. As estrogen declines, the body produces less collagen and joint lubrication, which can lead to inflammation and stiffness. Add in stress, sleep changes, or simply the natural wear and tear of life, and our joints begin to speak up.
But here’s the good news: you can take back comfort. With a few mindful practices—alongside healthy lifestyle choices—joint pain can be eased, and movement can feel light and joyful again.
Why Joints Need Extra Care in Menopause
Less estrogen → more inflammation: Estrogen helps protect cartilage and bone. When levels drop, inflammation can rise.
Stress and fatigue: Cortisol (the stress hormone) makes joint pain worse, while poor sleep reduces the body’s ability to recover.
Lifestyle shifts: More sitting, less stretching, and less movement all stiffen the body.
Think of menopause as a signal: your body is asking for new ways of being cared for.
Simple Everyday Helpers
Nutrition: Anti-inflammatory foods like berries, nuts, olive oil, and fatty fish help calm the body.
Hydration: Water keeps the joints lubricated and moving smoothly.
Supplements: Vitamin D, magnesium, and omega-3s may support joint and bone health (check with your doctor).
Breathwork: The Fastest Way to Release Tension
Breathing deeply isn’t just about oxygen—it’s medicine for your joints and nervous system.
Belly Breathing: Place a hand on your belly, inhale slowly, and feel it rise. This calms the nervous system and relaxes muscles around the joints.
Extended Exhale: Inhale for 4 counts, exhale for 6–8. This lowers stress and reduces the body’s pain sensitivity.
Cooling Breath (Shitali): Roll your tongue into a tube, inhale through it, exhale through the nose. Wonderful for cooling inflammation and calming hot flashes.
Meditation: Calming the Mind, Softening the Body
Pain feels sharper when the mind is tense. Meditation helps rewire how the brain experiences pain.
Body Scan: Gently move your awareness through your body, noticing areas of tension, then letting them soften.
Compassion Practice: Place a hand on the joint that hurts and send it kindness—this simple gesture reduces inner resistance and helps healing.
Mindful Movement: Even during daily walks, notice the rhythm of steps and breath. This shifts focus away from discomfort into flow.
Yoga: Gentle Movement for Freedom in the Joints
Yoga is a perfect ally for menopause because it combines breath, movement, and mindfulness. Even short practices help joints stay flexible, muscles strong, and the mind calm.
A few joint-friendly poses:
Cat–Cow: Increases spinal mobility and eases back and shoulder stiffness.
Supported Bridge Pose: Strengthens hips and glutes while releasing tension from the lower back.
Seated Side Bend (in a chair or on the floor): Opens the ribs, waist, and spine with gentleness.
Ankle Rotations & Wrist Circles: Small, daily movements that keep blood flowing to smaller joints.
Restorative Yoga with Props: Deep relaxation where the body can release inflammation naturally.
A Gentle Daily Ritual
🌅 Morning: 5 minutes of belly breathing + a few gentle stretches.
☀️ Midday: Chair yoga or a walk with mindful breath.
🌙 Evening: Restorative pose (Legs Up the Wall) + body scan meditation for deep rest.
Closing Thought
Menopause invites us to listen more carefully to the body. Joint pain is not just a nuisance—it’s a message to slow down, soften, and care for yourself in a new way. With breathwork, meditation, and yoga, you can create a body that feels supported and a mind that feels at peace.
✨ At ValU Within, we create safe and empowering yoga practices for women in transition. You don’t need to suffer through joint pain—there are tools to help you feel free, flexible, and deeply connected to your body again.